Sphenopalatine Ganglion Block for the Treatment of Headache and Facial Pain
Below is the abstract of the study A Novel Revision to the Classical Transnasal Tropical Sphenopalatine Ganglion Block Treatment of Headache and Facial Pain the study addresses the use of the Tx360® Nasal Applicator and it's effectiveness in clinical testing. This study has been printed by the Pain Physicians Journal: Offical Journal of the American Society of Interventional Pain Physicians.
The study concludes that the relief experienced by patients from the techniques used by the MiRx Protocol significantly reduces migraine and head pain. Also the ease of the Tx360® proved to be an excellent method of application for pain specialists, the board also concluded that the they believe the Tx360® could be used in the busiest of primary care and emergency department settings. The SPG block with the Tx360® provides for a fast, inexpensive, easy-to-use intervention in a variety of environments.
To read the full study Click Here.
November/December 2013 – Vol 1 Issue 6
ABSTRACT
2013;16;E769-E778. A Novel Revision to the Classical Transnasal Topical Sphenopalatine Ganglion Block for the Treatment of Headache and Facial Pain
Case Series
Kenneth D. Candido, MD, Scott T Massey, MD, Ruben Sauer, MD, Raheleh Rahimi Darabad, MD, and Nebojsa Nick Knezevic, MD, PhD
BACKGROUND
The sphenopalatine ganglion (SPG) is located with some degree of variability near the tail or posterior aspect of the middle nasal turbinate. The SPG has been implicated as a strategic target in the treatment of various headache and facial pain conditions, some of which are featured in this manuscript. Interventions for blocking the SPG range from minimally to highly invasive procedures often associated with great cost and unfavorable risk profiles.
OBJECTIVE: The purpose of this pilot study was to present a novel, FDA-cleared medication delivery device, the Tx360® nasal applicator, incorporating a transnasal needleless topical approach for SPG blocks. This study features the technical aspects of this new device and presents some limited clinical experience observed in a small series of head and face pain cases.
STUDY DESIGN: Case series.
SETTINGS: Pain management center, part of teaching-community hospital, major metropolitan city, United States.
METHODS: After Institutional Review Board (IRB) approval, the technical aspects of this technique were examined on 3 patients presenting with various head and face pain conditions including trigeminal neuralgia (TN), chronic migraine headache (CM), and post-herpetic neuralgia (PHN).
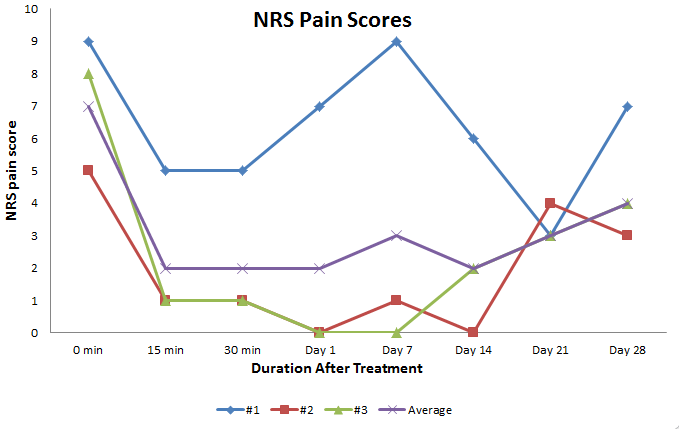
The subsequent response to treatment and quality of life was quantified using the following tools: the 11-point Numeric Rating Scale (NRS), Modified Brief Pain Inventory — short form (MBPI-sf), Patient Global Impression of Change (PGIC), and patient satisfaction surveys. The Tx360® nasal applicator was used to deliver 0.5 mL of ropivacaine 0.5% and 2 mg of dexamethasone for SPG block. Post-procedural assessments were repeated at 15 and 30 minutes, and on days one, 7, 14, and 21 with a final assessment at 28 days post-treatment. All patients were followed for one year. Individual patients received up to 10 SPG blocks, as clinically indicated, after the initial 28 days.
RESULTS: Three women, ages 43, 18, and 15, presented with a variety of headache and face pain disorders including TN, CM, and PHN. All patients reported significant pain relief within the first 15 minutes post-treatment. A high degree of pain relief was sustained throughout the 28 day follow-up period for 2 of the 3 study participants. All 3 patients reported a high degree of satisfaction with this procedure. One patient developed minimal bleeding from the nose immediately post-treatment which resolved spontaneously in less than 5 minutes. Longer term follow-up (up to one year) demonstrated that additional SPG blocks over time provided a higher degree and longer lasting pain relief.
LIMITATIONS: Controlled double blind studies with a higher number of patients are needed to prove efficacy of this minimally invasive technique for SPG block.
CONCLUSION: SPG block with the Tx360® is a rapid, safe, easy, and reliable technique to accurately deliver topical transnasal analgesics to the area of mucosa associated with the SPG. This intervention can be delivered in as little as 10 seconds with the novice provider developing proficiency very quickly. Further investigation is certainly warranted related to technique efficacy, especially studies comparing efficacy of Tx360 and standard cotton swab techniques.
To read the full study Click Here.